Personalized Medicine: How tailored treatment works in real life
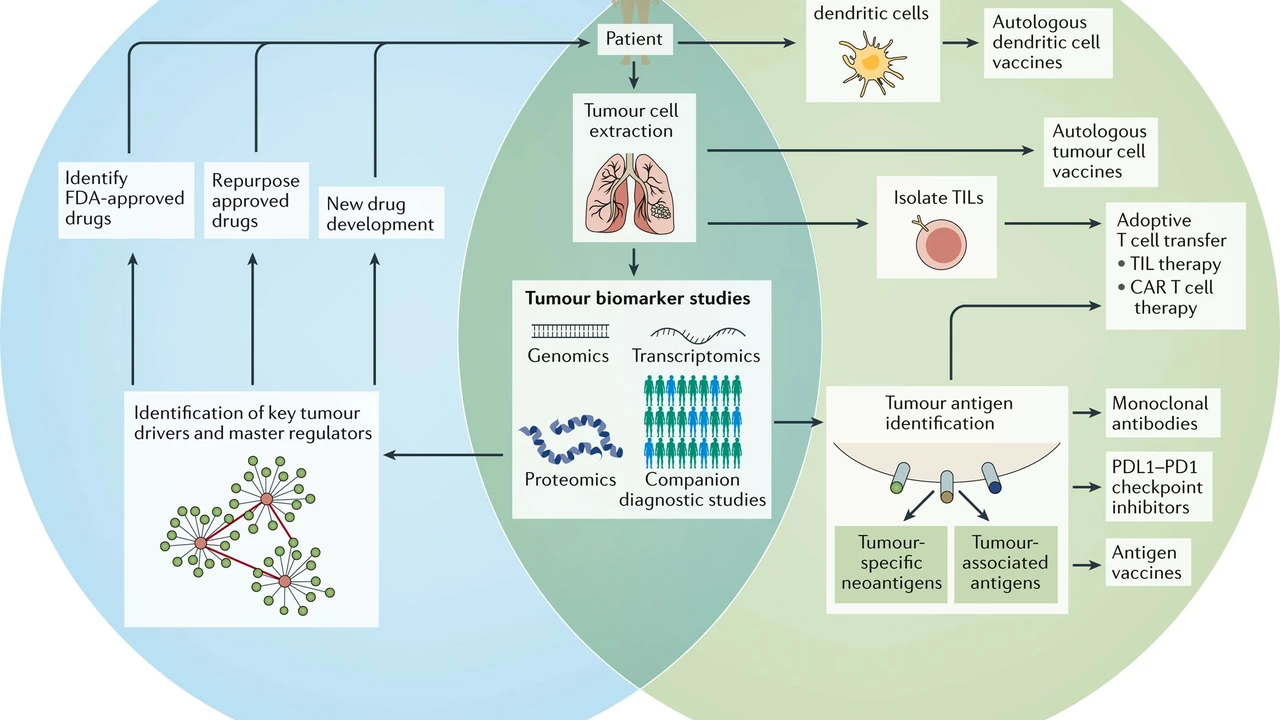
Personalized medicine means choosing tests and treatments that fit the person, not just the disease. That can be a genetic test that changes a drug dose, a targeted cancer drug that attacks a specific mutation, or picking an antidepressant based on how your body breaks down medicines. The goal is simple: better results with fewer side effects.
Clear examples you’ll recognise
Cancer care shows this best. Drugs like ibrutinib work for blood cancers with certain molecular patterns. If a lab finds that pattern, a doctor can pick ibrutinib instead of older chemo. That’s faster benefit and often fewer side effects. Another common example: warfarin dosing. Tests for VKORC1 and CYP2C9 genes can explain why one person needs a tiny dose while another needs more. Same drug, very different plan.
Pharmacogenomics also affects everyday meds. Some people are "fast metabolizers" of codeine and get too much morphine from it. Others are "slow" and get no pain relief. Tests for enzymes like CYP2D6 or CYP2C19 help predict that — and help your doctor choose safer alternatives.
When personalized medicine helps — and when it won’t
Use it when test results change the plan. That includes many cancers, some blood thinners, and certain psychiatric drugs. It also helps if you’ve had bad reactions to medicines, or if a family member shows a genetic disorder that affects drug response.
But it’s not a magic fix. Tests cost money, not every drug has a clear genetic rule, and evidence keeps changing. Insurance may not cover every test. Also, genetic results don’t replace good clinical judgment — they’re one tool among many.
Practical tips: bring a full list of medicines to your appointment, mention any strong reactions you had, and ask if a pharmacogenetic test makes sense for your case. If you get tested, ask for clear steps: how results change dosing, alternatives, and follow-up monitoring. Protect your data — ask how results are stored and who can see them.
Want more reading? Check our MedixRX Pharmaceutical Guide posts that dig into personalized topics. Read “Exploring the Pros and Cons of Ibrutinib Therapy for Cancer Treatment” for a cancer-drug example, “Genetics and Blood Clots: Understanding the Connection” to see how inherited genes affect clot risk, or articles on drug alternatives and side-effect profiles when treatment needs a personal touch. These pieces show how tests and choices work in real patients.
Personalized medicine is already changing care. It doesn’t apply to everything, but when used right it saves time, avoids harm, and makes treatments fit the person — not the average patient on a leaflet.
The Role of Personalized Medicine in Neuroblastoma Treatment
In my recent research, I've delved into the role of personalized medicine in treating neuroblastoma, a type of cancer that mostly affects children. Personalized medicine tailors treatment based on the genetic makeup of the cancer, offering a more effective approach. This targeted therapy means that the treatment can specifically attack cancer cells, reducing harm to healthy cells and potentially leading to better outcomes. The hope is that personalized medicine will not only increase survival rates but also reduce the long-term side effects often experienced by survivors. It's a promising field that could revolutionize how we treat neuroblastoma and other cancers.