Poor Muscle Control – Understanding the Basics
When dealing with poor muscle control, the inability to coordinate or sustain muscle movements effectively. Also known as muscle weakness, it often signals underlying health issues. A common manifestation is muscle spasms, involuntary contractions that disrupt normal movement. These spasms can be triggered by neurological disorders, conditions that affect the brain, spinal cord, or peripheral nerves such as Parkinson’s disease, multiple sclerosis, or peripheral neuropathy. Another key driver is medication side effects, drug‑induced changes that impair motor function, especially with statins, corticosteroids, or certain anti‑seizure meds. Understanding these links helps you pinpoint why your muscles feel out of sync.
How Different Factors Shape Poor Muscle Control
First, muscle spasms act as a red flag. They’re not just random twitches; they often reflect electrolyte imbalances, dehydration, or over‑use of a muscle group. When spasms become frequent, they reduce the range of motion and make everyday tasks feel exhausting. Second, neurological disorders disrupt the signal pathways that tell muscles when to contract or relax can cause both spasticity and flaccidity. For example, a stroke may damage the motor cortex, leading to poor coordination on one side of the body. Third, many prescription drugs alter calcium handling or nerve transmission, creating a side‑effect profile that includes weakness or tremor. Recognizing medication‑related muscle issues is crucial because a simple dosage adjustment or switch can restore function.
Third, the bladder is not immune to control problems. bladder muscle spasms, involuntary contractions of the detrusor muscle often accompany poor overall muscle control, especially in conditions like overactive bladder or spinal injuries. These spasms can cause urgency, leakage, and discomfort, adding another layer of complexity to daily life. Addressing bladder issues often involves pelvic floor therapy, medications, or lifestyle tweaks, all of which intersect with broader muscle‑control strategies.
Finally, lifestyle and metabolic health play supporting roles. Chronic kidney disease can lead to secondary hyperparathyroidism, which weakens bones and muscles, while chronic lung diseases such as COPD increase systemic inflammation that dampens muscle performance. Even nutritional gaps—low vitamin D, magnesium, or protein—can tip the balance toward weakness. By looking at the whole picture—spasms, nervous system health, drug regimens, bladder function, and metabolic status—you get a roadmap for targeted interventions.
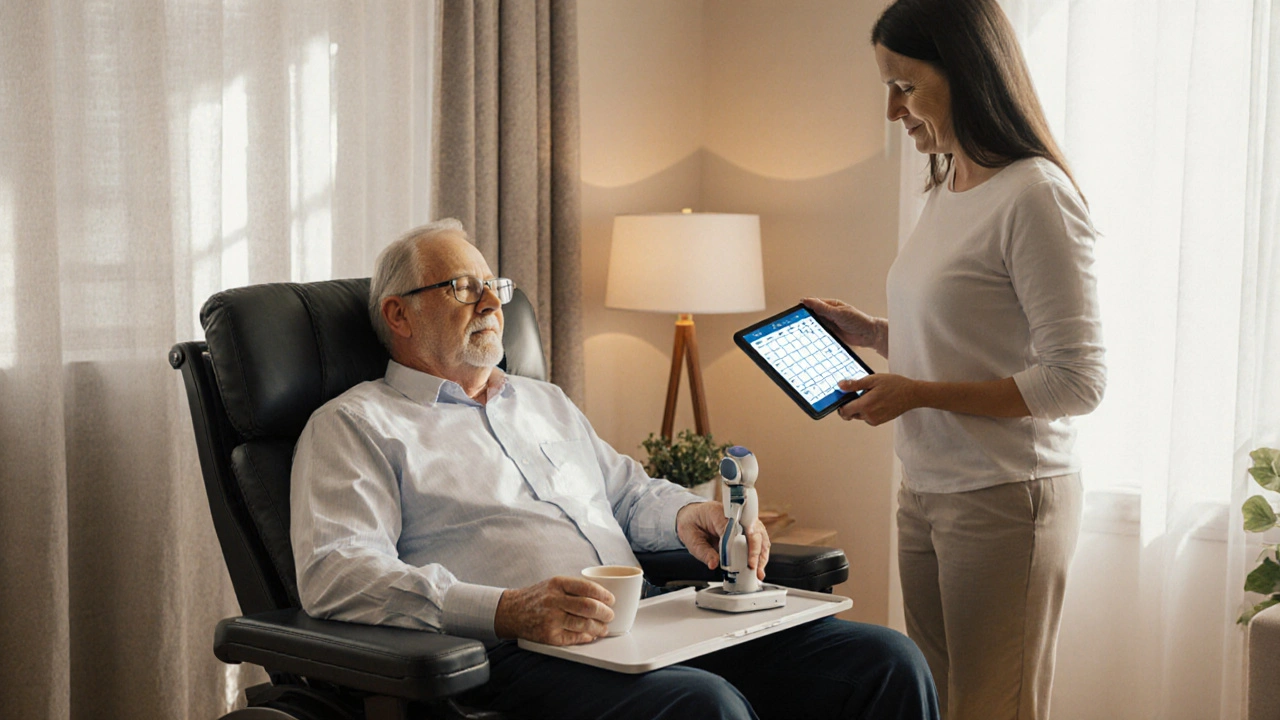
Below you’ll find a curated set of articles that dive deeper into each of these angles, from identifying specific drug side‑effects to managing bladder muscle spasms and tackling underlying neurological causes. Ready to explore practical tips and expert‑backed guidance? Scroll down to discover the resources that will help you regain better muscle control.
Effective Fatigue Management Strategies for Those with Poor Muscle Control
Learn practical ways to reduce fatigue for people with poor muscle control, covering energy conservation, assistive tech, sleep hygiene and caregiver tips.