Therapeutic Equivalence: What It Means and Why It Matters for Your Medications
When you hear therapeutic equivalence, the official determination that two drugs produce the same clinical effect and safety profile in patients. Also known as bioequivalence, it's the reason your pharmacist can legally swap your brand-name pill for a cheaper generic without asking your doctor. This isn’t marketing fluff—it’s science backed by the FDA, and it affects every prescription you fill. If two drugs are therapeutically equivalent, they have the same active ingredient, strength, dosage form, and route of administration. More importantly, they work the same way in your body. No guesswork. No risk. Just the same result at a fraction of the cost.
Therapeutic equivalence doesn’t just apply to simple pills. It covers complex products too, like inhalers, injectables, and even topical creams. For example, if you’re using an asthma inhaler, the generic version must deliver the exact same amount of medicine to your lungs as the brand name, down to the micron. The FDA tests this with real human studies—measuring how much drug enters your bloodstream and how fast it works. If the numbers match within strict limits, the generic gets an Therapeutic Equivalence rating, often marked as "AB" in the Orange Book. This rating system is what pharmacies and insurers rely on to approve substitutions. Without it, you’d be stuck paying brand prices even when cheaper options exist.
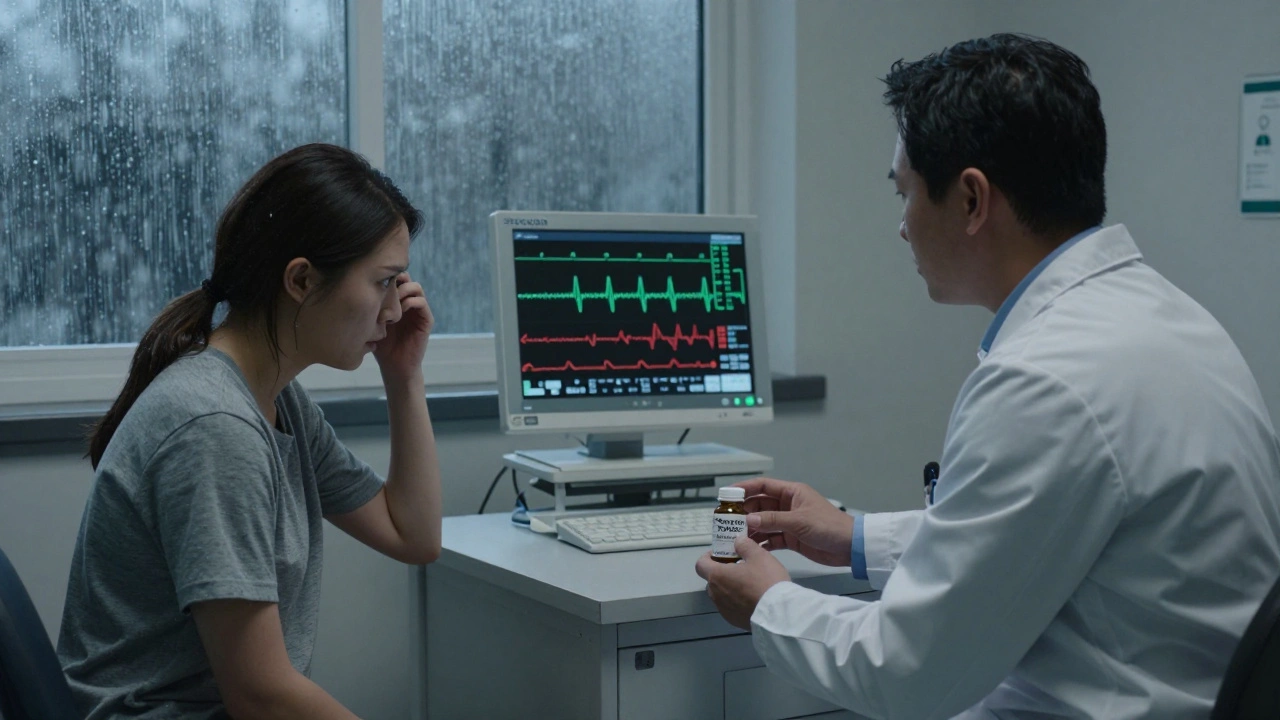
But therapeutic equivalence isn’t automatic. Some drugs—like warfarin, levothyroxine, or narrow-therapeutic-index medications—require extra scrutiny because tiny differences can cause big problems. That’s why not all generics are treated the same. The FDA keeps close watch on these, and sometimes even approved generics aren’t automatically interchangeable. You might notice your pharmacist asking if you’re okay with switching. That’s not because they’re unsure—it’s because they’re following the rules to keep you safe.
Understanding therapeutic equivalence helps you ask the right questions. If your prescription is switched to a generic, you can ask: "Is this rated AB?" If you feel different after the switch, it’s worth talking to your doctor—not because the generic is likely broken, but because individual reactions vary. Some people respond better to one manufacturer’s version than another, even if both are FDA-approved. That’s why the system allows for exceptions when needed.
Behind every generic drug that’s therapeutically equivalent is a long chain of testing, regulation, and transparency. The Hatch-Waxman Act made this system possible, and today, over 90% of U.S. prescriptions are filled with generics because of it. This isn’t about cutting corners—it’s about making quality care affordable. Whether you’re managing high blood pressure, diabetes, or allergies, therapeutic equivalence ensures you’re not paying more for the same medicine.
Below, you’ll find real-world examples of how this plays out—from how generic combination products are approved to why some people still hesitate to switch, even when it’s safe. These stories aren’t about theory. They’re about people who saved hundreds a year, avoided side effects, or finally got their meds covered by insurance—all because therapeutic equivalence works.
Medical Society Guidelines on Generic Drug Use: What Doctors Really Think
Medical societies have clear but differing positions on generic drug substitution. While most generics are safe, experts warn against switching for drugs with narrow therapeutic indices like seizure medications. Learn why doctors make these calls and what you should know.